Genital Surgery in Delhi
TrueFunction MtF SRS/GCS Surgery
TrueFunction GCS/SRS surgery is summed up in two main words
- Removal
- Reconstruction
If you had the chance of pre-puberty HRT, the only thing you will need is FtM SRS/GCS.
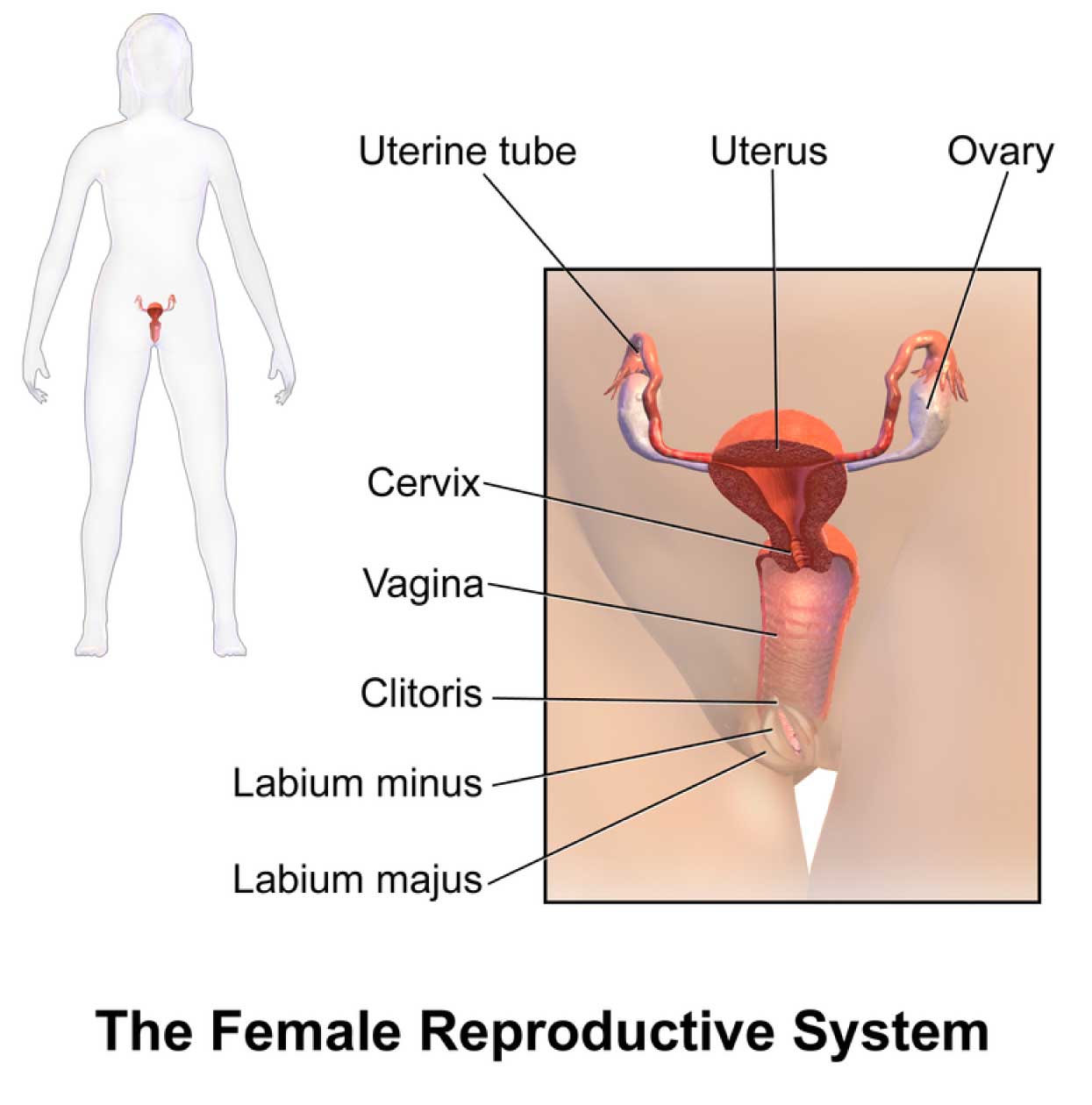
The female genital is much more complex than its male counterpart on the inside, this is where most of the basic GCS/SRS steps will be taking place. Let us take a look at the internal structures and the ways, sequences, and possibilities to have them removed first.
Then let us have a look at how the male genital will be reconstructed. After that, let us evaluate if these steps are truly independent or if these steps should be seen and treated as one single process, that should be performed in one go.
The chronological removal steps to take would be these:
- Laparoscopic removal of the ovaries and the fallopian tubes (Bilateral Salpingo-Oophorectomy/Ovarectomy or BSO)
- Laparoscopic removal of the uterus (Hysterectomy)
- Removal of the vagina (Vaginectomy)
The removal of the ovaries and the fallopian tubes, as well as the uterus, can be a very useful step to enhance HRT since your body doesn’t have to fight estrogen and progesterone production anymore. Therefore, any kind of menses and menses pain will be gone once the ovaries, the fallopian tubes, and the uterus are gone. This in turn will greatly enhance your quality of life.
When performing BSO, the logical and sensible thing to do is to remove the uterus at the same time because no (fertilized) egg can make itself at home there for 9 months.
These are the main reasons why BSO and uterus removal usually are performed together and why we highly advise them to be performed in one session.
What about the vagina?
Since Vagina removal/Vaginectomy is surgically interconnected with TLH/BSO (Total laparoscopic uterus and ovaries removal), it is best if performed together. One important aspect at this point becomes urethral elongation/extension more precisely Olmec’s TrueShape Urthral Masculinization which should take place immediately prior to vaginectomy. The vaginal tissues are utilized to make the most suitable natural lining for the urethra along with vaginal muscle usage for urethra reconstruction. Once the urethral extension is done, vaginal removal surgery is completed.
Is Simple Clitoris Release surgery considered a GCS/SRS surgery?
For us here at Olmec, the answer is no.
Simple Release surgery is when the testosterone-enlarged (virilized) clitoris gets freed from all its surrounding tissue and gets transformed into a clitpen without a shaft – the clitpen has more projection and more prominence, and it has the ability to erect. The urethra, labia majora, and vagina stay untouched. The clitpen needs to be freed from the labia minora though. Urination will happen through the regular biological urethral opening. The vagina is still functional and open.
TrueFunction MiniMG (Miniature Male Genital) SRS/GCS
Unfortunately, this GCS/SRS is oftentimes falsely labeled as Metoidioplasty.
In medical terms, medoidioplasty is the process of the construction of a mini-penis – nothing more and nothing less.

Do you have to be so serious about terminology?
Bear with us – we believe you will easily understand the reason why as soon as we explain it.
General Info on TrueFunction MiniMG GCS/SRS
Dr. Kaushik’s favorite FtM surgery is the MiniMG GCS/SRS.
The reasons for that are manifold:
- BSO, uterus removal, and vagina removal are surgically interconnected and rely on each other to be performed in one go to achieve the best possible result.
- Vagina removal and TrueFunction Urethra Lengthening as well as TrueFunction Urethra Masculinization are surgically interconnected steps in Dr. Kaushik’s TrueFunction MiniMG.
- Metoidioplasty – the creation of the mini penis – should be performed alongside the TrueFunction Urethral Lengthening.
- Surgery time is relatively short (around 5 hours), the complication rate is minimal, recovery is rather quick, and sensation, as well as function, are usually excellent for a complete MiniMG.
- FtM genital transformation is complete in one session.
Should you not want a complete MiniMG for whatever reasons, basically all steps can be performed separately, but it is not a good idea.
The steps are:
- Laparoscopic ovary and fallopian tube removal (BSO)
- Laparoscopic uterus removal (Hysterectomy)
Separating steps 1 and 2 will double anesthesia costs and surgery costs – and that simply doesn’t make sense. - TrueFunction vagina removal (Vaginectomy) which then requires the vagina to be closed
In Dr. Kaushik’s TrueFunction Vagina Removal, the removal of the uterus and the removal of the vagina are surgically connected. Separating these steps is possible, but the best result will be achieved when they are performed together. - TrueFunction urethra lengthening and TrueFunction urethra masculinization –
TheTrueFunction urethra lengthening needs vagina mucosa tissue for the urethra – and the TrueFunction urethra masculinization needs a vagina muscle flap to achieve the “squeeze-the-last-drop” effect of a regular male genital. The vaginal vestibul glands – namely the Skene glands and Bartholene’s glands – will be removed. - TrueFunction metoidioplasty – creating the mini-penis shaft using labia minora tissue
The mini penis shaft out of labia minora needs labia majora fat and labia majora fascia to be properly created around the enlarged and connecting-tissue-freed clitoris and the newly created TrueFunction urethra. - Creating a scrotal sac out of labia majora tissue (Scrotoplasty).
As you can see now, so many of the MiniMG steps depend on another step to be performed. That is the reason why proper terminology is so important. You as the patient and Dr. Kaushik need to know exactly what you are talking about when discussing your surgery.
TrueFunction MiniMG (Full or Partial MiniMG) GCS/SRS
At first, laparoscopic removal of the ovaries, fallopian tubes, and the uterus (TLH with BSO – Total Laparoscopic Hysterectomy with Bilateral Salpingo-oophorectomy), takes place. Dr. Kaushik again improved current procedures with his own handwriting. TrueFunction Vagina Removal to prevent fistula formation after uterus removal and vagina removal is one major improvement.
Before vagina removal, he performs his unique TrueFunction Urethra Lengthening that includes a vagina mucosa graft for urethra lengthening and a TrueFunction Urethra Masculinization that uses a vaginal muscle flap to give you the “squeeze-out-the-last-drop of pee” experience, just like it is for every guy.
On top of this, Dr. Kaushik improved his TrueFunction Urethral Lengthening in such a way, that possible future catheterization will work – instead of oftentimes ending up in a dead-end-street pouch.
You will have a catheter for a minimum of 10 days to allow for your new urethra to heal properly.
Dr. Kaushik will create a scrotal sac out of the labia majora tissue next if the patient opts to do so. This TrueFunction Scrotoplasty will have to heal first before the testicular implants can be added after all scrotal sac sutures have properly healed.
Will I be able to pee while standing after MiniMG?
That depends on a lot of factors like body weight, fat in the pelvic area, and maybe your willingness to pull your pants down further than just opening the zipper (decreases the distance for peeing while standing) when you pee while standing.
In general, here at Olmec more than 80% of our patients can empty urine while standing after MiniMG.
What about my sexual pleasure after MiniMG?
Our patients report excellent function, sexual arousal, and orgasm after MiniMG GCS/SRS. The great benefit of the MiniMG procedure is the very low complication rate, great sensation, and excellent function for the length available.
Sexual intercourse will not be possible with a MiniMG-penis. Oral sex, however, is reported as a wonderful and pleasureable experience for both partners.
TrueFunction Phalloplasty (Full Penis Reconstruction)
Without a doubt, phalloplasty is the most complex GCS/SRS for any surgeon to perform.
The challenges of phalloplasty are:
- it is the riskiest FtM GCS/SRS
- it is a very long surgery – usually +9 hours
- new structures have to be reconstructed that are not there yet, mostly out of what tissue is available in a patient
- has the highest complication rate of any GCS/SRS – namely 10% on average
- penile implant complication rate is around 50% – due to malfunction, infection, detachment issues, or the implant damaging surrounding tissue
- aesthetic results cannot be compared to a natural phallus/ penis – if your partner is keen on a natural penis, he or she will propably be disappointed – and so, in turn, will you
Some of the issues you raise here are the same for MiniMG GCS/SRS also, so why mention it here?
Yes, that is correct.
But please remember this one thing: MiniMG surgery is a relatively short 5-6 hour single procedure with a complication rate of close to zero. And most of what can be achieved for a TS*male in terms of form and function is achieved with MiniMG – simply smaller in size.
Phalloplasty is a very long surgery. Complication rate with urethra elongation is quite high, sensation and sexual pleasure oftentimes will decrease for the tip of your neopenis. Complication rate with semi-rigid or hydraulic penile implants is quite high, aesthetics is not very close to a natural penis – and all of this comes with very long recovery times and a very high price tag.
Visit our Before+After FtM GCS/SRS gallery to see results of phalloplasties perofred by Dr. Kaushik to see if your expectations will be met.
Please make very sure you understand all of the risks and potential gains.
Make sure you are clear on what your expectations are and what Dr. Kaushik can achieve for you.
Weigh all information thoroughly and properly before you decide to go forward with this procedure and all consequences that may come with it.